Understanding Regulatory Compliance in Healthcare

Regulatory compliance in healthcare shapes every patient experience, guiding how medical teams handle sensitive data and deliver care. Here is what might surprise you. A single failure to follow these rules can cost healthcare providers millions in fines and even loss of licensing. Most people think compliance is just another box to check but it is actually the backbone that keeps patients safe and builds trust in medical organizations.
Table of Contents
- Defining Regulatory Compliance In Healthcare
- The Importance Of Regulatory Compliance In Healthcare
- Key Regulations Governing Healthcare Compliance
- Challenges In Achieving Regulatory Compliance
- Future Trends In Regulatory Compliance For Healthcare
Quick Summary
| Takeaway | Explanation |
|---|---|
| Regulatory compliance ensures patient safety. | Compliance creates standards that minimize medical errors and consistently improve care quality. |
| Non-compliance leads to severe repercussions. | Consequences include financial penalties, legal challenges, and damage to reputation and trust. |
| Comprehensive strategies support compliance management. | Organizations should integrate technology, training, and monitoring to enhance adherence to regulations. |
| Technological advancements shape future compliance. | Evolving regulations will address AI, cybersecurity, telehealth, and data interoperability needs. |
| Patient-centric regulations will become essential. | Future compliance will focus on personalized approaches that meet individual patient needs and enhance care delivery. |
Defining Regulatory Compliance in Healthcare
Regulatory compliance in healthcare represents a comprehensive framework of rules, standards, and protocols designed to ensure patient safety, protect sensitive medical information, and maintain ethical standards across medical organizations. Research from the National Institutes of Health demonstrates that these regulations are critical for maintaining high-quality patient care and organizational integrity.
Core Components of Healthcare Compliance
Healthcare regulatory compliance encompasses multiple interconnected domains that organizations must carefully navigate. The primary components include:

- Patient Privacy Protection: Ensuring confidential medical information remains secure under regulations like HIPAA
- Clinical Standards: Maintaining evidence-based treatment protocols and quality care benchmarks
- Ethical Practice Guidelines: Implementing transparent medical procedures and preventing potential misconduct
These frameworks are not merely bureaucratic requirements but fundamental mechanisms for protecting patient rights and establishing trust within the healthcare ecosystem. Organizations must develop robust internal systems that can systematically track, verify, and document their adherence to these complex regulatory requirements.
Legal and Financial Implications
Non-compliance can result in significant consequences for healthcare providers. Potential penalties include substantial financial fines, potential loss of medical licensing, legal action, and reputational damage. Healthcare organizations must invest in comprehensive compliance management strategies that integrate technological solutions, staff training, and continuous monitoring.
By proactively addressing regulatory requirements, healthcare providers can transform compliance from a potential liability into a strategic advantage. This approach not only mitigates risks but also demonstrates an organization’s commitment to maintaining the highest standards of patient care. Learn more about modernizing healthcare dispatching to enhance your compliance strategies and operational efficiency.
The Importance of Regulatory Compliance in Healthcare
Healthcare regulatory compliance transcends mere legal obligation, serving as a critical mechanism for protecting patient welfare, maintaining organizational integrity, and fostering trust within the medical ecosystem. Research from the National Institutes of Health underscores the fundamental role these regulations play in safeguarding patient interests and maintaining high-quality healthcare delivery.
Patient Safety and Quality Assurance
Regulatory compliance directly impacts patient safety by establishing standardized protocols that minimize medical errors and ensure consistent care quality. Healthcare organizations must implement comprehensive systems that:
- Continuously monitor and assess clinical practices
- Validate medical professional credentials
- Maintain rigorous documentation and reporting standards
- Implement robust quality control mechanisms
These mechanisms create a structured environment where patient safety becomes a proactive priority rather than a reactive response. By establishing clear guidelines and accountability frameworks, regulatory compliance helps prevent potential medical mistakes and promotes a culture of continuous improvement.
Financial and Reputational Risk Management
Non-compliance carries substantial financial and reputational risks for healthcare organizations. Potential consequences include significant monetary penalties, legal challenges, loss of professional licensing, and erosion of patient trust. Learn more about preventing healthcare fraud to understand the critical importance of maintaining stringent compliance protocols.
Healthcare providers must view regulatory compliance as a strategic investment rather than a bureaucratic burden. By developing robust compliance strategies that integrate advanced technological solutions, comprehensive staff training, and proactive monitoring, organizations can transform potential risks into opportunities for demonstrating professional excellence and commitment to patient care.
Key Regulations Governing Healthcare Compliance
Healthcare regulatory compliance involves navigating a complex landscape of federal, state, and local regulations designed to protect patient rights, ensure quality care, and maintain ethical standards. The U.S. Department of Health and Human Services provides comprehensive guidance on the critical regulations that shape the healthcare industry.
Critical Federal Regulations
Several foundational regulations form the backbone of healthcare compliance in the United States. The most significant include:
- HIPAA (Health Insurance Portability and Accountability Act): Protects patient medical information privacy and establishes security standards for healthcare data
- EMTALA (Emergency Medical Treatment and Active Labor Act): Ensures patients receive emergency medical treatment regardless of ability to pay
- ACA (Affordable Care Act): Expands healthcare access and implements quality improvement standards
These regulations create a comprehensive framework that healthcare providers must meticulously follow. Each regulation addresses specific aspects of patient care, from information protection to treatment accessibility, requiring organizations to develop robust compliance strategies.
The following table summarizes the critical federal regulations governing healthcare compliance, highlighting their main focus and how they impact healthcare organizations.
| Regulation | Main Focus | Impact on Healthcare Organizations |
|---|---|---|
| HIPAA (Health Insurance Portability and Accountability Act) | Protects patient medical information privacy and data security | Requires secure handling of patient information and implementing privacy measures |
| EMTALA (Emergency Medical Treatment and Active Labor Act) | Ensures emergency treatment regardless of ability to pay | Mandates emergency care provision to all patients, affects operations and policies |
| ACA (Affordable Care Act) | Expands access and implements quality standards | Drives quality improvements and access initiatives, requires ongoing compliance monitoring |
Credentialing and Professional Standards
Professional credentialing represents another critical component of healthcare regulatory compliance. Healthcare organizations must verify and maintain rigorous standards for medical professionals, ensuring they meet established qualifications and continue to demonstrate professional competence. Check out our guide on navigating credentialing challenges to understand the complexities of maintaining professional standards.
Compliance is not a static process but a dynamic, ongoing commitment.

Healthcare providers must continuously update their understanding of regulatory requirements, implement comprehensive training programs, and develop technological solutions that support consistent adherence to these complex and evolving standards.
Challenges in Achieving Regulatory Compliance
Regulatory compliance in healthcare presents a complex landscape of evolving requirements that challenge even the most sophisticated medical organizations. Research published in the International Journal of Business and Social Research reveals the multifaceted nature of these compliance challenges, highlighting the intricate balance between maintaining patient safety and navigating administrative complexities.
Technological and Data Security Obstacles
Healthcare organizations face significant challenges in protecting patient data and maintaining robust technological infrastructures. Key technological compliance challenges include:
- Implementing secure electronic health record (EHR) systems
- Protecting patient information from cybersecurity threats
- Ensuring seamless data interoperability across different healthcare platforms
- Maintaining up-to-date security protocols that meet federal regulations
These technological challenges require continuous investment in advanced security measures and ongoing staff training. Organizations must develop comprehensive strategies that anticipate potential vulnerabilities and proactively address emerging technological risks.
Regulatory Interpretation and Implementation
One of the most significant challenges in healthcare compliance stems from the complex and often ambiguous nature of regulatory requirements. Healthcare providers must constantly interpret and implement regulations that can be nuanced and subject to frequent changes. Explore our guide on navigating credentialing challenges to understand the intricacies of maintaining professional standards.
Successful compliance requires more than simple rule-following. It demands a proactive approach that combines legal expertise, technological innovation, and a deep commitment to patient care. Healthcare organizations must develop adaptive compliance strategies that can quickly respond to regulatory changes while maintaining the highest standards of patient safety and organizational integrity.
This table outlines the primary challenges healthcare organizations face in achieving regulatory compliance, along with corresponding examples from the article.
| Challenge | Example from Article |
|---|---|
| Technological and Data Security Obstacles | Securing EHR systems, protecting against cybersecurity threats |
| Regulatory Interpretation and Implementation | Navigating ambiguous and frequently changing regulatory requirements |
| Data Interoperability Needs | Ensuring seamless data exchange across healthcare platforms |
| Continuous Training and Monitoring | Ongoing staff training and proactive compliance management |
Future Trends in Regulatory Compliance for Healthcare
Healthcare regulatory compliance is rapidly evolving, driven by technological advancements, changing patient expectations, and increasingly complex healthcare delivery models. Research examining the historical trajectory of healthcare policy demonstrates the ongoing transformation of regulatory frameworks to address emerging challenges in patient care and data management.
Technological Integration and AI Governance
The future of healthcare compliance will be fundamentally shaped by technological innovations and their corresponding regulatory requirements. Key emerging trends include:
- Artificial intelligence and machine learning governance protocols
- Advanced cybersecurity standards for healthcare data protection
- Regulatory frameworks for telehealth and remote patient monitoring
- Comprehensive guidelines for interoperable health information systems
Healthcare organizations must develop adaptive strategies that anticipate technological shifts while maintaining rigorous compliance standards. This requires continuous investment in technological infrastructure and proactive regulatory engagement.
Personalized Compliance and Patient-Centric Regulations
Regulatory frameworks are increasingly moving towards more personalized and patient-centric approaches. Compliance will no longer be a one-size-fits-all model but a dynamic, adaptive system that responds to individual patient needs and emerging healthcare delivery models. Learn more about upcoming healthcare trends to understand how regulatory compliance is transforming.
The future of healthcare compliance demands a holistic approach that balances technological innovation, patient privacy, and organizational flexibility. Successful healthcare providers will be those who view regulatory compliance not as a burden, but as a strategic opportunity to enhance patient care, improve operational efficiency, and build trust in an increasingly complex healthcare ecosystem.
Take Control of Healthcare Compliance and Patient Logistics
Navigating regulatory compliance in healthcare is a complex and high-stakes responsibility. The article highlights challenges like protecting patient privacy, ensuring documentation accuracy, and minimizing costly errors. These requirements can overwhelm any organization, putting patient safety and your reputation at risk. Your team strives for high standards, but fragmented communication, manual processes, and evolving regulations make it hard to keep up. Imagine what you could do if compliance felt effortless—and you knew your operations were always audit-ready.
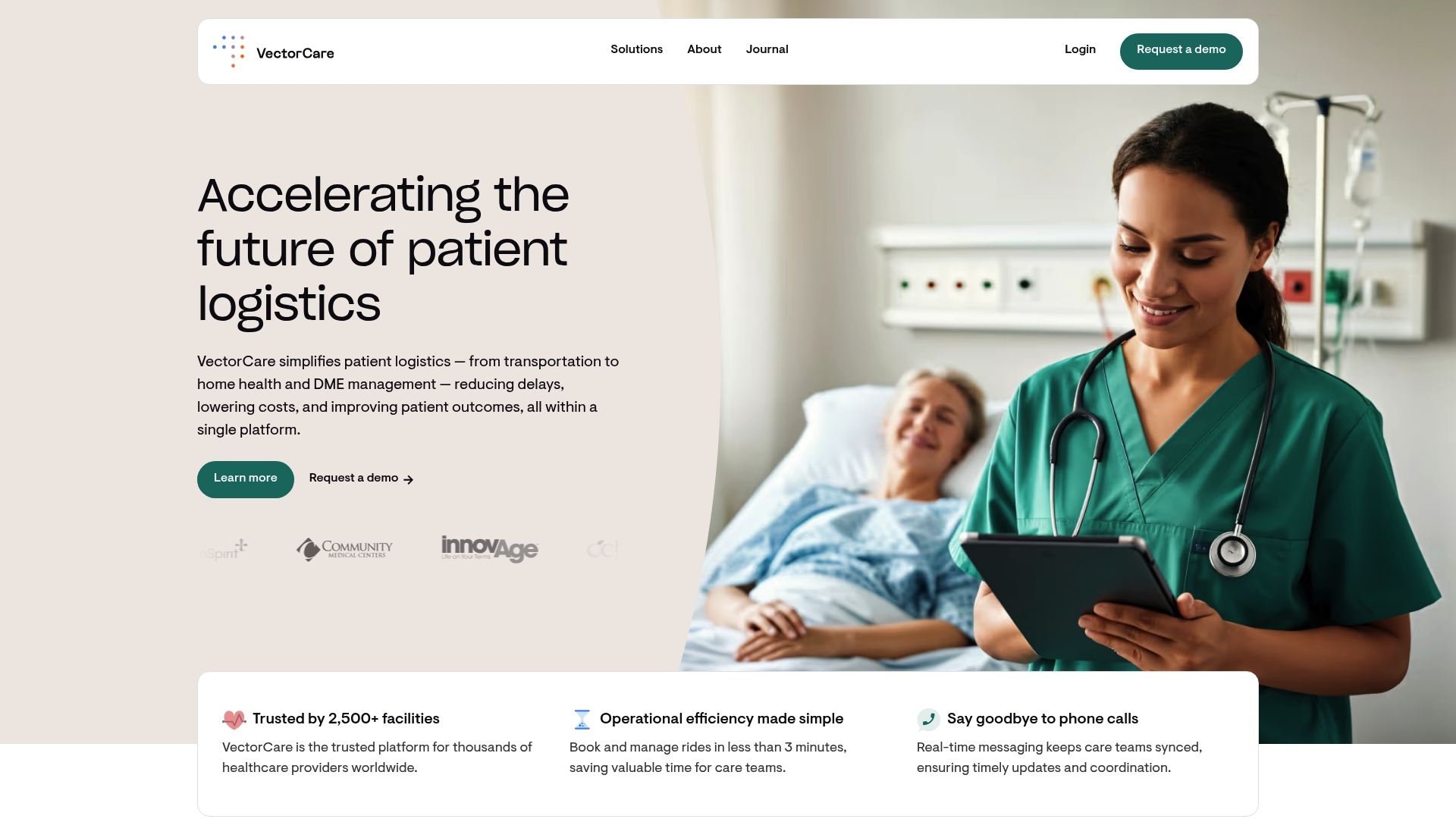
See how VectorCare’s digital platform helps healthcare leaders turn regulatory challenges into a strategic advantage. Automate key workflows, coordinate with providers and vendors in real time, and gain deep insights into compliance metrics across patient transport, home health, and equipment delivery. The result is reduced delays, lower costs, and most importantly, improved patient outcomes.
Learn how VectorCare empowers you to simplify compliance, achieve safer care coordination, and scale your impact. Experience the future of healthcare logistics—visit our site and discover how your organization can thrive today.
Frequently Asked Questions
What is regulatory compliance in healthcare?
Regulatory compliance in healthcare refers to the framework of rules, standards, and protocols established to ensure patient safety and the integrity of medical organizations, protecting sensitive medical information and ensuring ethical practices.
Why is regulatory compliance important in healthcare?
Regulatory compliance is crucial for protecting patient welfare, ensuring high-quality healthcare delivery, and maintaining organizational integrity. It helps minimize medical errors, build patient trust, and avoid financial penalties for non-compliance.
What are the key components of healthcare compliance?
Key components of healthcare compliance include patient privacy protection, adherence to clinical standards, and implementation of ethical practice guidelines, ensuring that healthcare organizations follow necessary regulations to safeguard patients.
What are the potential consequences of non-compliance in healthcare?
Non-compliance in healthcare can lead to severe consequences, including substantial financial penalties, legal challenges, loss of medical licensing, and reputational damage, impacting both the organization and the trust of patients.